Washington State has life and death public health policy choices to make. We were leading the nation in making some of these choices, but a review of models shows why Governor Inslee had to take additional steps immediately to avoid much greater loss of life and spread of COVID19.
As both a legislator and public health faculty member at UW School of Public Health, I’ve been reviewing models to help both the public and our state decision makers understand what choices we should be making, and the dire consequences of delay. Some of the models have been reported, but not widely here in Washington.
There are some articles and commentaries saying we should have just increased testing and quarantine. But our State – like the entire nation – continues to face tremendous obstacles to increase testing. I spent the early part of last week working with the UW and fellow 46th District legislators to assist UW to dramatically increase testing capacity (UW had the fastest turnaround on tests in US). This week we have doubled daily capacity. However, we are at about 40% of where we need to be to test the first-responders, health care and congregate care workers, ill patients in congregate care. The obstacles include the failure of the federal government to deliver supplies and leaving states to compete with one another.
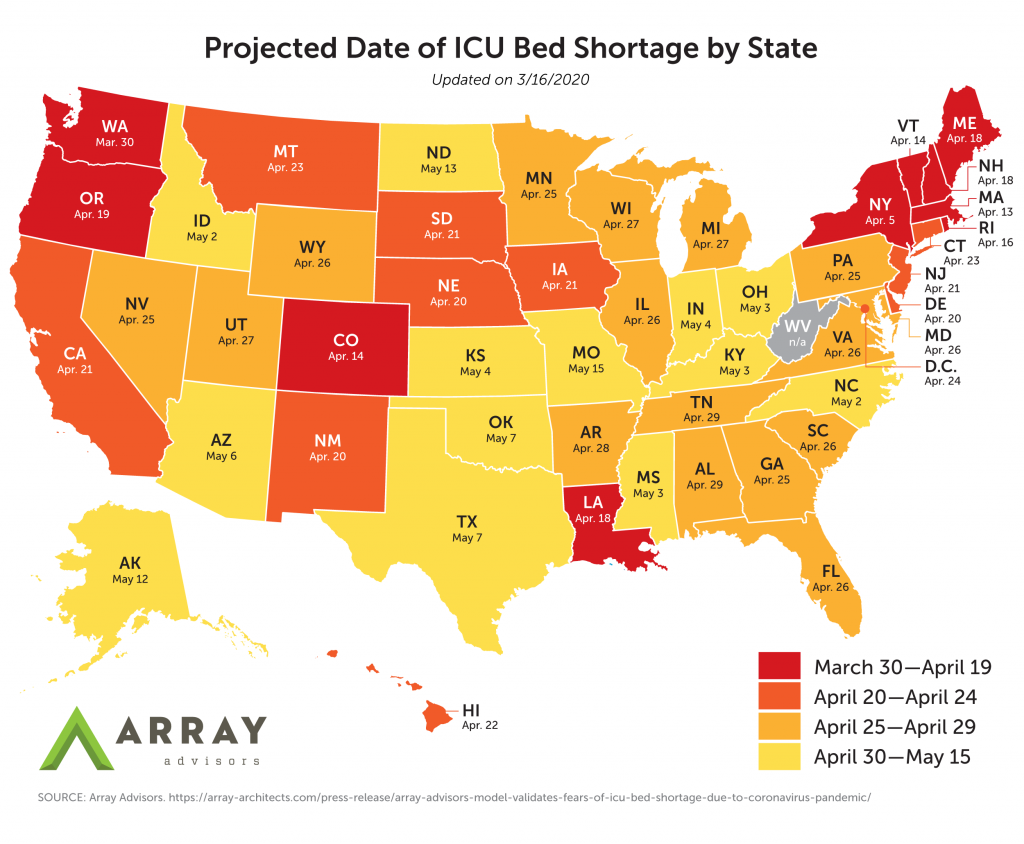
If Washington State did not adopt additional mandatory measures to prevent social interaction, increase testing, quarantine people who have had contact with those who may be infected, and increase hospital capacity, various models predict we would overwhelm our hospital bed, especially ICU / critical care bed, capacity around April 1st.
If people are not treated in ICU with ventilators, etc., the fatality rate will rise dramatically.
This is why canceling elective surgeries was essential. We must now work on developing surge capacity for our health care system (perhaps we will realize for longer term policy that we must invest far more to train health care professionals to meet our recognized shortage).
Graphics accompanying various models illustrate why these steps and why the Governor’s Order for people to stay home except for essential work and essential shopping were absolutely necessary.
If we had taken no action at all in Washington, the mortality projection from one model with easily understandable graphics, was for 116,000 deaths in Washington and a peak of 157,000 hospitalizations.
Washington state has under 12,000 hospital beds and under 1,500 ICU critical care beds. Our hospital and ICU bed occupancy rate is typically about 65%. (hospital bed data from Harvard Global Health Institute and T.H. Chang School of Public Health; Covidactnow.org Washington model has slightly lower hospital bed figures). Other models predict that we would continue to exceed hospital capacity for a year or more.
If we only adopted 3 months of mostly voluntary “social distancing,” as in many states, that same model with easily understandable graphics shows that Washington State would exceed our hospital capacity on March 30th and not return to being below capacity until May 13 with a peak of 65,536 hospitalizations required.
If we adopt California level mandatory “shelter in place” for three months, that same model predicts Washington would be at hospital bed capacity from approximately April 13 to approximately May 1. Projected mortality: 16,000 deaths rather than 66,000 deaths from laxer “social distancing” measures (and 7,962 hospitalizations predicted). Model and data from CovidActNow.org Click here to see the easily understandable interactive graphic showing the consequences of different policy choices for our State: https://covidactnow.org/state/WA. You can also view the impacts of choices for every other state on their home page.
This graph is viewed better online for interactions and updates at https://covidactnow.org/state/WA).
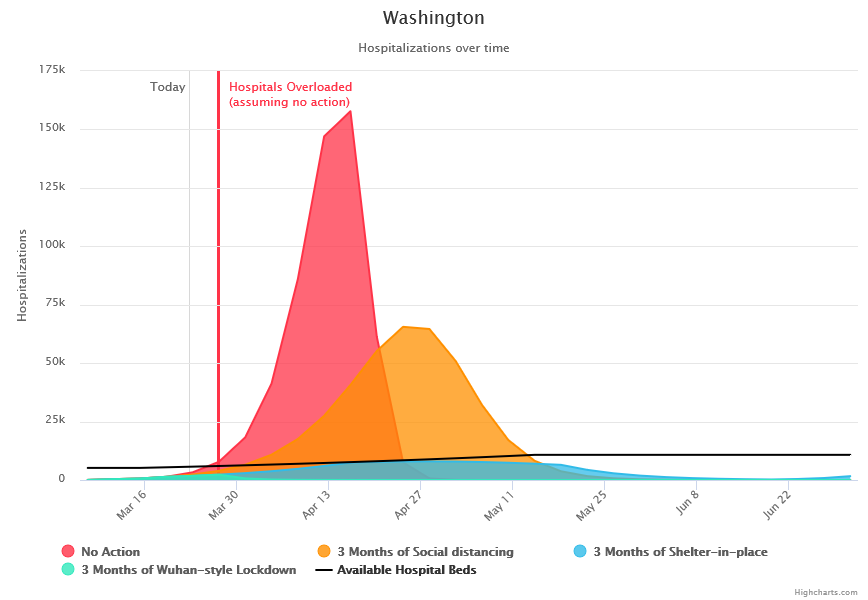
Credit: covidactnow.org
Note CovidActNow assumption for Hospital beds in Washington: 10,765.
Fatality rate increases if adequate hospital beds are not available. All assumptions and data available at https://docs.google.com/document/d/1ETeXAfYOvArfLvlxExE0_xrO5M4ITC0_Am38CRusCko/edit
Another model finds: “Washington, a state with the second-most confirmed cases in the country as of Monday afternoon, is expected to hit its ICU capacity by March 30. New York, a state with over 930 cases, is expected to hit its capacity by April 5.”
Click on map to view in browser or expand.
Experts view the model developed and published last week by the Imperial College (UK) as the most reliable. CovidActNow utilizes key data from their modeling, which was done for nation-wide impacts in Great Britain and the US, and provides easily understood state by state graphic depictions of the consequences of decisions to “flatten the curve” to reduce the “reproduction number” (R0) – the number of infections each infected person transmits to others.
The Imperial College Model for the US shows the relative effectiveness of key policy choices:
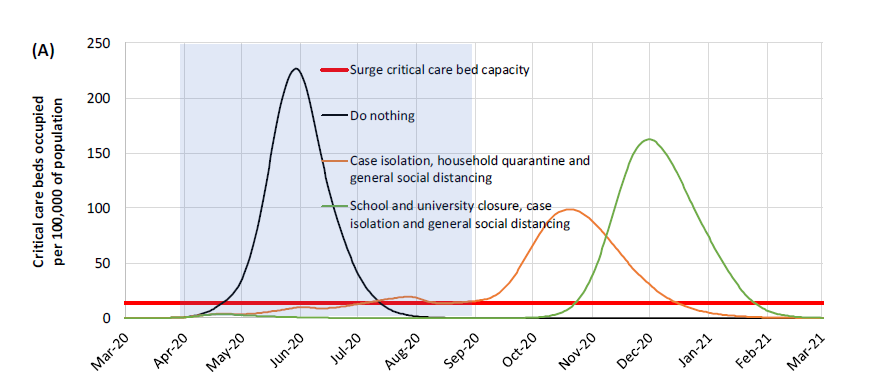
Credit: Imperial College London
We can relax from lock-down to isolation if we find through expanded testing, that the rate, and extent of, infection is being controlled. But if we find that the current rate of spread from each infected individual (R0) is higher and we have greater incidence, it will be too late to effectively prevent an overwhelming number of infections with any further delay in ordering home stay and these other measures.
Here is the conclusion of the Imperial College report:
We find that that optimal mitigation policies (combining home isolation of suspect cases, home quarantine of those living in the same household as suspect cases, and social distancing of the elderly and others at most risk of severe disease) might reduce peak healthcare demand by 2/3 and deaths by half. However, the resulting mitigated epidemic would still likely result in hundreds of thousands of deaths and health systems (most notably intensive care units) being overwhelmed many times over. For countries able to achieve it, this leaves suppression as the preferred policy option.
We show that in the UK and US context, suppression will minimally require a combination of social distancing of the entire population, home isolation of cases and household quarantine of their family members. This may need to be supplemented by school and university closures, though it should be recognized that such closures may have negative impacts on health systems due to increased absenteeism. The major challenge of suppression is that this type of intensive intervention package – or something equivalently effective at reducing transmission – will need to be maintained until a vaccine becomes available (potentially 18 months or more) – given that we predict that transmission will quickly rebound if interventions are relaxed. We show that intermittent social distancing – triggered by trends in disease surveillance – may allow interventions to be relaxed temporarily in relative short time windows, but measures will need to be reintroduced if or when case numbers rebound.
In the absence of any control measures, the Imperial College paper predicts that there would be 2.2 million deaths in the US. This estimate does not include additional deaths due to lack of hospital capacity for other illness and accidents.
This data on hospitalization and mortality does not factor in lack of adequate PPE, testing and hospital equipment or staffing. Shortages for each would increase the mortality rate in addition the lack of hospital beds. Thus, the lower mortality rate assumed for having adequate hospital beds may not hold if hospitals are not able to be staffed or equipped properly. This illustrates the importance of cancelling elective surgeries and dedicating PPE, test capacity and staffing.
We are all going to continue to be in this together. This will not end in a week or two. No one is immune from the Corona virus. Many people in other regions of the US and here, including younger people, think that they are not at high risk. With a high school student in our isolated household, I understand the frustrations and desires to return to normalcy.
You can help by sharing well reviewed research and data from reliable sources to help others understand that even young people are at significant risk. Teachers and faculty might ask students to review these models and discuss them as part of at home learning.
Perhaps teachers and faculty might have students discuss a comparison of the models I’ve linked here to alternate policy choices such as this view from the Lt. Governor of Texas on Monday in support of relaxing measures, as reported in USA Today
The lieutenant governor of Texas argued in an interview on Fox News Monday night that the United States should go back to work, saying grandparents like him don’t want to sacrifice the country’s economy during the coronavirus crisis.
Republican Lt. Gov. Dan Patrick, 69, made the comments on Fox News’ “Tucker Carlson Tonight” after President Donald Trump said he wanted to reopen the country for business in weeks, not months.
Patrick also said the elderly population, who the Centers for Disease Control and Prevention said are more at risk for COVID-19, can take care of themselves and suggested that grandparents wouldn’t want to sacrifice their grandchildren’s economic future.
These policy choices are not just about the risk of you and your family getting COVID19. Please consider that your isolation, support for these steps, and voicing your opinion on whether the federal government should assist more directly, will save the lives of people you know and love.
Rep. Gerry Pollet